Windy Cole (director of Wound Care Research, Kent State University College of Podiatric Medicine, Cleveland, USA) presented the first case—to her knowledge—to document healing in a calciphylaxis wound with the use of continuous topical oxygen therapy (cTOT) at the Symposium on Advanced Wound Care Fall 2020 meeting (SAWC; 4–6 November, online). Guided by her experience, she concluded that topical oxygen therapy offers an effective, non-invasive wound treatment that may speed healing in chronic non-healing wounds of various aetiologies that were recalcitrant to other advanced wound therapies. “Finding creative ways to navigate this current health care crisis [the COVID-19 pandemic] is essential to help mitigate risk for vulnerable patients with advanced comorbidities,” she said.
Historically, the treatment for calciphylaxis is not well-standardised, she explained, and involves various medications and wound care modalities. In the case presented, a 56-year-old patient with diabetes and end-stage kidney disease, who had been on peritoneal dialysis for 14 months, had a painful, discoloured lesion on the left lateral calf that had been present for three weeks. This was proven by biopsy to be a calciphylaxis lesion.
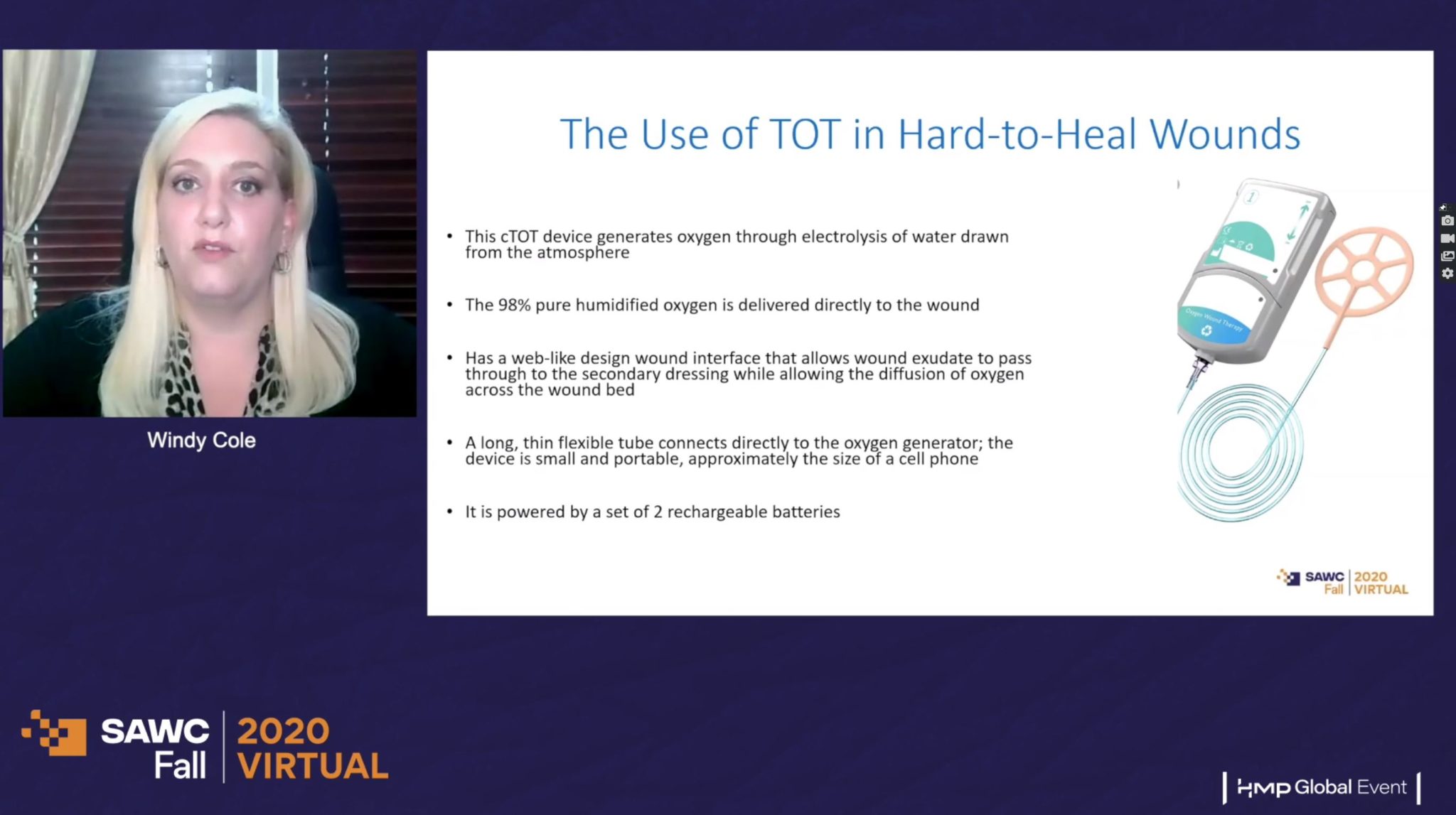
In this patient case, the continuous topical oxygen therapy relied on patient self-application. Detailing how the continuous topical oxygen therapy (cTOT) device worked, Cole explained that it generates oxygen through electrolysis of water drawn from the atmosphere. The 98% pure humidified oxygen is delivered directly to the wound, continuously (“so twenty-four hours a day, seven days a week”) and has a web-like design at the wound interface that allows wound exudate to pass through to the secondary dressing while allowing the diffusion of oxygen across the wound bed. A long, thin, flexible tube connects directly to the oxygen generator. “The device is small and portable, approximately the size of a small cell phone, and it can actually be strapped to the lower leg and hidden under a skirt or a pant [trouser] leg,” she described, and is powered by a set of two rechargeable batteries.
“We wanted to make certain that we protected this high-acuity patient from the COVID-19 pandemic, and try to keep her safe at home as much as possible and limit her exposure at the wound care centre or the hospital, so I decided to initiate the topical oxygen therapy with her, and the patient did her own dressing changes twice a week.” Cole and colleagues conducted weekly telemedicine visits to monitor wound progress.
The wound was completely resolved within nine weeks of therapy without complications, and the patients was able to be placed back on the kidney transplant list.
“Now, more than ever, innovative therapies paired with alternative treatment sites of service such as telemedicine are vital to help mitigate risk for vulnerable patients with advanced comorbidities,” she reflected. “The use of topical oxygen therapy for future treatment of calciphylaxis and other hard-to-heal wounds is an area that warrants additional study.”
Continuous topical oxygen therapy heals otherwise non-healing wounds in pilot case series
Cole and colleagues additionally conducted a prospective, single centre, single-arm pilot case series with the aim of determining the effects of weekly continuous topical oxygen therapy on wound tissue perfusion, as measured with a near-infrared spectroscopy device (NIRS).
She explained how this camera was used to measure the proportion of oxygen bound to haemoglobin: the NIRS measures the absorbance of light in the near-infrared spectrum, and allows for the calculation of oxygen saturation of the wound tissue. This allows clinicians to get a better idea of the functional blood flow into the tissues.
Five participants over the age of 18 with lower extremity wounds that had not healed more than 50% in 30 days were included in this study. After signing the informed consent form, a standard wound assessment was performed with baseline wound measurements and NIRS imaging. Active continuous topical oxygen therapy was initiated in the wound, and weekly NIRS images were obtained to track tissue oxygenation. Wound measurements were also taken weekly. All patients were seen for six weekly visits, or until wound healing was achieved, whichever occurred first.
The cases
Cole then talked SAWC delegates through each case. In each of the five patients under investigation, the long-lasting, non-healing wound had failed to improve with standard-of-care treatment options, but did heal after a few weeks of continuous topical oxygen therapy—within the 12-week study period, “which is pretty impressive”, Cole commented.
“Every single patient had a decrease in total wound area at each weekly visit, and then also, at each weekly visit, we did see an increase overall in the oxygen saturation, as tested with the near-infrared spectroscopy camera,” Cole related. As the oxygen saturation in the wound increased, the total wound area decreased, leading Cole to muse: “so they did seem to be mutually beneficial to the patient.”
Case one was a 91-year-old man with a 22-week history of a non-healing ulcer following a below-the-knee amputation on the left leg. He also had peripheral arterial disease (PAD) and non-insulin-dependent diabetes. His wound had previously been dressed with alginate and collagen, but these had not helped. Upon initial presentation, the wound measured 1.5cm x 1.6cm x 0.2cm, and was covered in eschar (dead tissue cast off from the surface of the skin). At baseline, the wound had a 54% oxygen saturation; at three weeks, the wound was healed, and the patient was sent to his orthotist to reconfigure his prosthetic so he could begin to walk again.
The second case was an 85-year-old woman with a trauma wound on the right lower leg that had not healed after eight weeks. Previous standard-of-care dressings, including collagenase ointment, alginate, and multilayer compression therapy had been used to no avail. Prior to beginning continuous topical oxygen therapy, the wound measured 4cm x 1.5cm x 0.1cm. At baseline, after debridement, oxygen saturation was 44%; after three weeks of topical oxygen therapy, this was 65%. In addition to this increased oxygenation to the wound, Cole recounted how the clinicians were also seeing more tissue formation; “the wound was responding very well to topical oxygen therapy”. After five weeks of this treatment, the wound was healed.
Case three was a 76-year-old man with a right leg venous ulcer of 54 weeks’ duration. The patient had venous insufficiency, psoriasis, osteoporosis, and pericarditis, which “all complicate healing,” in Cole’s words. Previous, failed wound management included multilayer compression dressings, antimicrobial creams, silver alginates, collagen, and amniotic tissue grafts. Prior to beginning continuous topical oxygen therapy, his wound measured 3.1cm x 3.2cm x 0.1cm. At baseline, tissue oxygen saturation was 58%; at three weeks, this had improved to 78%. “It kind of plateaued,” Cole noted, informing virtual conference attendees that at five weeks, oxygen saturation was 77%. “But, we saw him go on to complete healing in nine weeks of continuous topical oxygen therapy,” she added.
The fourth case was a 42-year-old woman with a 14-week-old diabetic foot ulcer on the left second toe. He had non-insulin-dependent diabetes, anxiety, obesity, depression, fatty liver, and sleep apnea, and had previous failed topical antimicrobial treatment and alginate dressing. At baseline, her wound was 0.7cm x 1cm x 0.1cm, with moderate peri-wound masceration, and an oxygen saturation of 72%. At three weeks, this increased to 87%, and the wound was healed at four weeks.
Finally, case five was an 85-year-old man with a left lower leg extremity venous leg ulcer of 62 weeks’ duration. “We had tried and failed all of our standard-of-care dressings and even some advanced modalities in our attempts to get this wound to heal,” Cole relayed: alginate, foam and compression dressings, iodine, silver dressings, collagen, medical-grade honey, and collagenase ointment were all unsuccessful. At baseline, the wound measured 9.2cm x 2.8cm x 0.2cm, and oxygen saturation was 65%. After three weeks of continuous topical oxygen therapy, this improved to 79%, and after five weeks, oxygen saturation had risen again to 83%. After 11 weeks, healing was complete.